Unveiling The Mind-Body Connection: Exploring Functional Medicine Approaches To Mood Disorders
If you’re reading this right now, odds are you know someone who has been diagnosed with or silently suffers from a mood disorder. In fact, you may have personally encountered a mental health condition of your own.
According to the World Health Organization (WHO), it was estimated 1 in 8 people globally had a mental health condition in 20221. The most common types of mental disorders include anxiety and depression. Other common mental health-related conditions include bipolar disorder, post-traumatic stress disorder (PTSD), schizophrenia, attention-deficit hyperactivity disorder (ADHD), and eating disorders.
Mental health conditions drastically change a person’s day to day life. This involves everything from physical, nutritional, and spiritual health, but also overall quality of life. Although treatment options have advanced in Western medicine, the prevalence of mood disorders continues to be on the rise. The recent global pandemic in 2020 made mood disorders, especially anxiety and depression, even more prevalent.
The most common treatment option for various mood disorders continues to be pharmaceutical medications. Antidepressants are one of the most common drug classes prescribed to Americans2. In fact, the Centers for Disease Control and Prevention (CDC) estimated that approximately 1 in 8 male and female Americans at least 12 years old have taken this type of medication. There is no denying that medication can be beneficial when prescribed and utilized appropriately. However, as the amount of prescribed antidepressants continues to increase, it begs the question– are we as a society continuing to work towards the root cause and relief of symptoms, or are we putting a “band-aid,” in the form of a pill, on the underlying issues that could be linked to a multitude of mood disorders?
In this e-book, we will dive into some of the most common mental health conditions: anxiety, depression, and bipolar disorder, and the research-based relationship functional medicine may play in the management and potential prevention of these conditions.
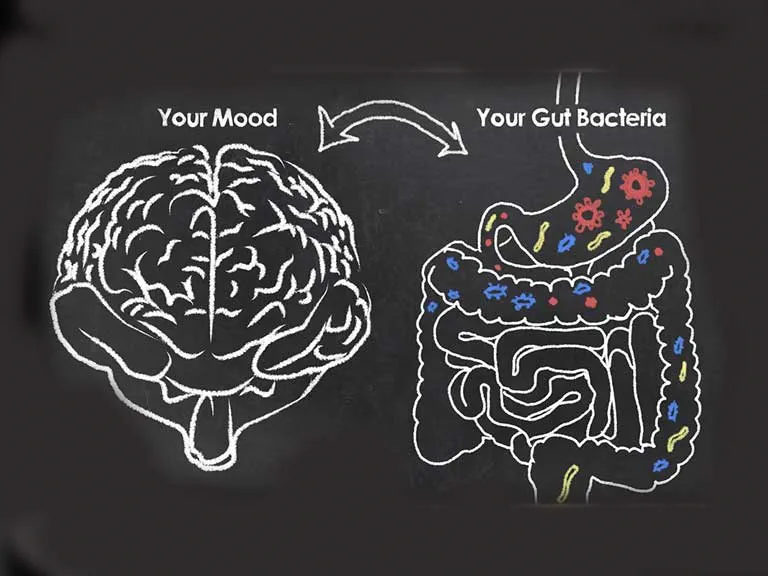
The Gut-Brain Connection
If you’ve been following me for quite some time, you know the gut is the main focus of my own health journey and the present focus of my career. Besides nutrient digestion and absorption, the gut has a LOT of important jobs, from thyroid health, immune function, and overall mood. The Gut-Brain Axis is the communication line between your gastrointestinal (GI) system and the brain. Each system has a direct impact on the other, meaning if one system is out of balance, the other will also suffer negative consequences.
Your gut microbiome is composed of both good and bad bacteria, as well as their genetic material. Different lifestyle factors, such as stress, poor diet, and medications, can have a negative impact on your microbiome over time. Instead of plentiful amounts of beneficial bacteria residing in your gut, the balance between beneficial and potentially harmful bacteria begins to shift. As the levels of bad bacteria begin to rise, your gut is at risk for developing intestinal permeability, or “leaky gut.” These gaps in the lining of your intestines can cause various toxins, such as heavy metals, harmful bacteria, and waste products, to sneak into your gut. As your intestinal lining becomes more permeable, this puts the gut, and for that matter the body as a whole, in a more inflammatory state.
If the gut is in an inflammatory state for a prolonged period, the body will ramp up its natural defense mechanism by releasing neurotransmitters and cytokines in an attempt to decrease inflammation. As these natural “fighters” begin to increase in number, they will also start to travel throughout the body systemically and cross the blood-brain barrier. Thus, the negative health state that started in the gut has now made a detrimental impact on the brain. Anxiety, depression, and memory recall have been linked to intestinal permeability.
In one research study, participants who were found to have higher levels of pro-inflammatory cytokines from a systemic stress response had increased states of anxiety and depression.
Although research continues to evolve in this area, there are some developing areas of interest in strengthening the Gut-Brain Axis. For one, probiotics (beneficial gut bacteria) seem to have a neuroprotective effect by blocking the firing of signals between your brain’s nerve cells (neurons) caused by a stress response. This in turn may potentially limit brain damage caused by an imbalanced microbiome. The exact mechanism, beneficial bacterial strains, and full impact are still being explored. In addition, taking a lifestyle modification approach first may also prevent the negative signs and symptoms of mood disorders, which we will discuss later on.
The Hypothalamic-Pituitary-Adrenal (HPA) Axis
In addition to the Gut-Brain Axis, another important pathway is the hypothalamic-pituitary-adrenal (HPA) axis. As the name suggests, this system involves the hypothalamus, pituitary gland, and adrenal glands.
In times of stress, whether it be emotional, physiological, or dietary stress, the HPA axis is turned on. The hypothalamus begins secreting hormones, thus encouraging the pituitary gland to release adrenocorticotropin hormone (ACTH)4. ACTH is a key hormone in encouraging cortisol to be released from the adrenal glands4. Cortisol, commonly referred to as the “stress hormone,” is largely responsible for our body’s stress response. We all need adequate amounts of cortisol to effectively respond to day to day stressors. However, if our stress response is constantly elevated (meaning we live in a constant state of stress), our cortisol levels will also stay elevated. Just like most things in life, there eventually comes a time when our adrenal glands get burnt out from constantly secreting cortisol. This can lead to something known as “adrenal fatigue.” Although not an official medical diagnosis, adrenal fatigue refers to a collection of symptoms including specific food cravings, low energy, and poor sleep hygiene.
In patients with mood disorders, elevated cortisol is seen to be a common occurrence. In addition, a poor ACTH response has been documented in major depressive disorder, one of the most common forms of depression. Although specific treatment options are still being actively researched, there is a direct correlation of HPA axis irregularities in mood disorders, specifically major depressive disorder.
Depression
Depression is one of the most common types of mood disorders. It is estimated that (at least, around, some sort of clarifying term) 5% of adults worldwide have some form of depression. The feeling of emptiness and loss of hope can bleed into every area of life, including nutrition, daily activities, social relationships, and physical health.
As mentioned above, antidepressants are one of the most common treatment options in Western Medicine. Although antidepressants may minimize symptoms and improve quality of life, these medications do not get to the root cause of the mood disorder, they don’t actually heal you from what was causing your depression in the first place.
 When looking inward at depression and its potential causes, we want to focus on three different aspects of one’s lifestyle: mental, physical, and nutritional. Over recent years, there has been increasing interest in non-medication treatments for depression. Specifically, therapy in its various forms has been shown to improve symptoms caused by depression, especially having a positive outlook on life. In addition, regular physical activity has been shown to minimize symptoms caused by non-severe depression. Movement is important!
When looking inward at depression and its potential causes, we want to focus on three different aspects of one’s lifestyle: mental, physical, and nutritional. Over recent years, there has been increasing interest in non-medication treatments for depression. Specifically, therapy in its various forms has been shown to improve symptoms caused by depression, especially having a positive outlook on life. In addition, regular physical activity has been shown to minimize symptoms caused by non-severe depression. Movement is important!
Anxiety
Another common mood disorder is anxiety. While there are several different types of anxiety, the most common symptoms include: fatigue, worry, difficulty focusing, disordered sleep, headaches, irritability, muscle aches, and unexplained pains. The severity of anxiety can occur on a spectrum, from occasional anxiety-ridden episodes to crippling anxiety that impacts day-to-day life.
Similarly to depression, medications are often sought out to help treat symptoms caused by anxiety. While medications do have their place and are necessary for some, pharmacological treatment does not get to the root cause of anxiety. From a functional medicine lens, getting to the root cause will help minimize, and potentially alleviate, anxiety-induced symptoms.
Neurotransmitters
For many years, there has been a scientific association with imbalanced neurotransmitters and most mood disorders. Neurotransmitters are the signaling molecules sent by neurons to other cells. Think of neurotransmitters as the “middleman” since they are signals sent from the presynaptic cell to the postsynaptic cell. With this in mind, let’s breakdown the four most common neurotransmitters:
- Dopamine : the “happy hormone”
- Function: important for the brain and the body to get you moving by supporting desire and executing daily tasks
- Food Sources: animal products, avocados, banana, beets, coffee, dark chocolate, dairy products (milk, cheese and yogurt)
- Acetylcholine: the memory neurotransmitter
- Function: works closely with the central nervous system (CNS) to promote muscle control, memory, attention, and autonomic body functions
- Food Sources: cod, quinoa, beef liver, egg, roasted chicken breast
- GABA: the calming neurotransmitter
- Function: this neurotransmitter works to limit anxiety and tenseness throughout the body
- Food Sources: beef liver, eggs, quinoa, broccoli, Brussel sprouts
- Serotonin: the “sleepy” neurotransmitter
- Function: plays a critical role in not only in sleep, but also in digestion, sex drive, mood, bone health, blood clotting
- Food Sources: Serotonin is not naturally found in foods. However one of the amino acids, tryptophan, can be converted to serotonin. Tryptophan-rich food sources include animal products (meat, poultry, and seafood), pineapple, tofu, nuts, and seeds
Neurotransmitters are key in making sure your body functions properly. If neurotransmitters are functioning at too high or too low of rates, this can have a direct impact on your body’s day to day operations. For example, low levels of GABA, an inhibitory neurotransmitter, have been linked to anxiety, depression, irregular sleep, irritability, and seizures. It is important to have adequate levels of neurotransmitters in order for the body to function properly.
In functional medicine, neurotransmitters are one of the first lab panels run in those experiencing various mood disorders. Ensuring dietary intake of the above precursors of neurotransmitters can also guarantee consistent levels of these important chemical messengers. If an imbalance of one of these neurotransmitters, especially GABA, is found, it is important to look at why this is occurring.
 First, an important body system to simultaneously analyze is the gut. The Gut-Brain Axis is just one important role the gut plays. In addition, the gut also produces many important metabolites. In fact, the majority of your body’s serotonin is produced in the gut8. Which means, if there is an underlying issue in the gut, such as leaky gut, gut dysbiosis, or immune irregularities, this will have a direct impact on neurotransmitter production. The lack of serotonin, and other neurotransmitters, will directly impact the brain’s functioning, which in turn can lead to an increasing severity of mood disorders over time.
First, an important body system to simultaneously analyze is the gut. The Gut-Brain Axis is just one important role the gut plays. In addition, the gut also produces many important metabolites. In fact, the majority of your body’s serotonin is produced in the gut8. Which means, if there is an underlying issue in the gut, such as leaky gut, gut dysbiosis, or immune irregularities, this will have a direct impact on neurotransmitter production. The lack of serotonin, and other neurotransmitters, will directly impact the brain’s functioning, which in turn can lead to an increasing severity of mood disorders over time.
Additionally, stress (in all of its many forms) can have an impact on neurotransmitter function. When it comes to stress, it is important to look at different lifestyle factors. Work, family, exercise, and other lifestyle factors all affect our body’s cortisol response. We all need adequate levels of cortisol to effectively combat day to day stressors. However, chronically elevated levels of cortisol can have a negative impact on neurotransmitter production. In addition, inflammation, whether specifically in the gut or throughout the whole body, can also have a detrimental impact on functioning neurotransmitters. Another factor that creates a stress state in the body is blood sugar imbalance. Blood sugar balance is critical in maintaining a steady state in the body. An imbalanced diet lacking nutrient-dense foods and an improper ratio of macronutrients (ie: heavy carbs) can lead to imbalances in blood sugar levels over time. These blood sugar imbalances (think of a rollercoaster constantly moving up and down) can impact other areas of our lives, including sleep. Sleep, and the body’s Circadian Rhythm, are two other important considerations in mood disorders.
Circadian Rhythm
Circadian Rhythm is an important process that we all can benefit from supporting on a daily basis. Circadian Rhythm is defined as a 24-hour cycle our bodies naturally follow that revolves around light9. This biological process relies on certain cues, such as light, temperature, and meal timing. Going way back to the beginning of time, our ancestors rose with the sun and fell asleep around the time the sun went down for the day. In addition, they were hunters and gatherers, allowing for consistent meal intake throughout the day. This allowed them not only to stay in tune with the patterns of nature, but also to keep their Circadian Rhythms in check.
Flash forward to today: most of us are not consistent with our sleep routines (also known as sleep-wake cycles) or our meal timing. In fact, it is estimated that 1 in 3 American adults are constantly sleep deprived. In addition, about half of American adults report not getting enough sleep and feeling tired at least three days of the week. These disruptions to our Circadian Rhythm cues can have a major impact on our day to day life. Over time, they can lead to increased risk for developing certain chronic health conditions, such as obesity, type 2 diabetes, and certain cancers.
There are several factors that can impact our Circadian Rhythms. First, hormones play a major role in regulating this cycle. Two key hormones play a role in our sleep wake cycle: melatonin and cortisol. Think of melatonin as the sleeping hormone, since it regulates sleep, and cortisol as the waking hormone, as it controls the timing of waking up and eating. The ratio of these hormones is constantly changing, depending on the time of day and certain lifestyle factors. However, if either of these hormones are out of balance, this can lead to irregular sleep patterns, such as sleeping during the day and trouble falling asleep or staying asleep at night.
A second factor is stress. Cortisol has already been discussed with the HPA Axis, but it is important to note just how impactful high stress hormone secretion is on the body. Regulating stress levels, whether they be emotional, dietary, or physical stressors, is key to restoring cortisol to baseline.
Another factor to consider is poor diet. As mentioned above, inconsistent meal timing and consuming the Standard American Diet (SAD) can not only impact internal stress, but also can throw our Circadian Rhythms out of whack. Our ancestors relied on natural, whole-food sources for nutrition, not processed items lacking nutrient density and found in a bag or box at a grocery store. In addition, inconsistent meal timing, including skipping meals or irregularly eating/snacking throughout the day, can also disrupt this biological clock.
Our nighttime routines are another factor that can impact our Circadian Rhythms. Instead of taking the time to wind down each night and limit screen time (also known as blue-light exposure), most of us find ourselves spending too much time on an electronic device and hastily trying to fall asleep each night. Blue-light exposure actually signals to our brains that it is still daytime and encourages our normal body processes that occur during the day to continue on well past the sun going down. The best way to limit blue-light exposure is to limit screen time at least 30 minutes to an hour before bed while using blue-light blocking devices, such as a quality pair of glasses throughout the day.
Not surprisingly, the gut also plays a role in Circadian Rhythm regulation. The Gut-Circadian Rhythm connection can be disrupted by three main aspects: gut dysbiosis, irregular eating patterns, and antibiotic use. Gut dysbiosis can signal to the Circadian Rhythm that something is off as far as gut microbiome composition of both good and bad gut bacteria. Antibiotic use, especially chronically, actually clears out both the good and bad bacteria in your gut, leading to decreased immunity and overall function of the beneficial bacteria.
Besides potentially modifying your nighttime routine and stress management, another beneficial lifestyle habit to make part of your routine is daily sunlight exposure. Some different ways to incorporate being outdoors into your day are reading, journaling, taking a walk, meditating, biking, or eating your meals outside. Although it is likely more feasible to get adequate sunlight in the summer months, it is also possible to get sunlight in the cooler months as well! Some great ways to do this include: red light therapy or a short morning walk or jog outdoors. One of the top things to avoid in the winter months is hibernating indoors. Even just 5-10 minutes of sunlight can help keep your Circadian Rhythm in check.
Key Nutrition Strategies
Now that we have discussed various mood disorders and the role functional medicine may play in managing these symptoms, let’s dive into some important nutritional components linked to improved signs and symptoms of said mood disorders. Please note, these strategies are not meant to completely cure or replace other lifestyle modifications, such as therapy.
Overall Diet Quality
Diet quality plays a huge role not only with our digestion and risk for various chronic diseases, but also our mood. As mentioned above, the Standard American Diet (SAD) is full of processed foods and lacks the nutrient variety that our body needs. In fact, multiple studies have studied the impact of the American diet on brain function. One study in particular found that high calorie foods (which are most commonly consumed as processed foods) decrease neuronal plasticity, a key component of learning and memory.
On the other hand, a randomized controlled trial (RCT) performed in 2019 focused on a Mediterranean-style diet for those with moderate to severe depression. A Mediterranean diet is well-known for being anti-inflammatory and involves consuming a variety of whole foods. After 12 weeks, participants who focused on the Mediterranean diet had improvement of symptoms using a standardized depression rating scale. This study emphasizes the importance of diet quality!
Choosing a variety of anti-inflammatory whole foods, such as fruits, vegetables, and minimally processed protein options, not only improves your gut, but also has a direct impact on your Gut-Brain Axis.
Key Food Groups to Try to Limit for Inflammation:
- Added sugars
- Processed foods (especially those with inflammatory seed oils)
Vitamin D
Vitamin D, also known as “the sunshine vitamin,” is another important micronutrient to include in the diet. Vitamin D can be obtained through the sun. However, it is estimated that at least 35% of American adults are deficient in Vitamin D13. Vitamin D has many important functions, including bone and muscle health, mood, and supporting energy levels. If deficient in Vitamin D, various symptoms can occur, including joint pain, muscle cramping, fatigue, and mood changes (including depression)13.
Several foods are common sources of Vitamin D, including: salmon, tuna, egg yolk, and mushrooms. For some people, supplementation of this vitamin may be necessary, especially if daily sunlight exposure is not an option. However, before beginning supplementation, it is critical to have your Vitamin D level checked through lab testing overseen by a licensed healthcare professional. After your Vitamin D level is established, you and your healthcare provider can determine whether supplementation is necessary.
Omega-3 Fatty Acids:
Omega-3’s are another important anti-inflammatory nutritional component. Two of the main types of omega-3’s, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) actually work to bring down the inflammatory response in the brain by decreasing several proinflammatory cytokines. These proinflammatory cytokines, if left unmanaged, have been linked to mood disorders, such as depression and anxiety.
One study on healthy American adults found that a daily dose of 5 grams of EPA + DHA combined reduced not only proinflammatory cytokines but also significantly reduced a critical fatty acid ratio, arachidonic acid (AA) to EPA15. The AA/EPA ratio is critical in measuring the levels of pro-inflammatory fatty acids, such as AA, to anti-inflammatory fatty acids, such as EPA.
Some of the common food sources of omega-3 fatty acids include: fatty fish, such as salmon, mackerel, tuna, and herring; avocados, and certain nuts and seeds, such as chia seeds. If these foods are not able to be consistently part of your diet, supplementation may be necessary. Similar to Vitamin D, it is important to check your fatty acid levels prior to supplementation to determine the dosage needed, as well as the AA/EPA ratio. This lab testing can be performed by a licensed healthcare professional, including a functional medicine practitioner.
B Vitamins:
There are a wide variety of B vitamins, each with their own unique purpose. The B vitamins specifically linked to brain health include: cobalamin (B12), pyridoxine (B6), thiamine (B1), and folate (B9)16. Let’s break each of these down into more detail:
-
- Vitamin B12
- Function: important in neurogenesis, homocysteine metabolism, overall cognition, and making the myelin sheath for neurons (remember those neurotransmitters?)
- Food Sources: meat, eggs, tempeh, dairy products, nutritional yeast
- Vitamin B6
- Function: important for making neurotransmitters, homocysteine metabolism
- Food Sources: legumes, fish, poultry, dark leafy greens, bananas
- Vitamin B1
- Function: brain glucose metabolism, protects cognitive function in times of stress; deficiency has been linked to dementia
- Food Sources: nuts, liver, rice, legumes, steak, tuna, and acorn squash
- Vitamin B12
- Vitamin B9
-
- Function: assists B12 in homocysteine metabolism, plays a part in making neurotransmitters, and helps repair neurons
- Food Sources: legumes, cauliflower, broccoli, dark leafy greens, liver, beets, brussel sprouts
Maintaining a nutrient-dense diet is critical to not only support your physical body, but also your mental state as well. Each of these micronutrients, in combination with an anti-inflammatory diet, can support a healthy mindset and minimize symptoms related to mood disorders. In summary, eating a wide variety of whole foods, moving your body daily, and taking care of your mind through daily mindfulness (including therapy!) all work together to achieve an overall healthy lifestyle.
Key Takeaways:
-
- Lifestyle factors, such as diet, exercise, and stress, play an important role in the management of mood disorders, such as anxiety and depression
- The Gut-Brain Axis is the communication line between your gastrointestinal (GI) system and the brain. If inflammation is found in the gut, this can impair the communication line with the brain, leading to potential mood disorders
- In times of stress, the hypothalamic-pituitary-adrenal (HPA) axis is turned on, leading to an eventual secretion of cortisol, the stress hormone. Over time, if cortisol levels remain chronically elevated, this can lead to adrenal fatigue.
- Regular physical activity, in combination with a balanced, whole-food diet, has been shown to improve symptoms brought on by depression.
- Neurotransmitters, such as dopamine, GABA, acetylcholine, & serotonin, are the “middleman” since they are signals sent from the presynaptic cell to the postsynaptic cell.
- Circadian Rhythm is the term used to describe our bodies’ daily rhythm, or biological clock, revolving around light. Daily light has been shown to have many benefits, including mood boosting.
-
- Some of the key nutritional components to consider in regards to mood disorders are: diet quality, vitamin D, omega-3 fatty acids, and certain B vitamins.
- Please note: this ebook is not intended to be medical advice, nor is it meant to treat, diagnose, or cure any injury or illness. It is for informational purposes only.
Click here to begin your journey with a Functional Medicine approach through Rachel Scheer Nutrition. We are here to answer your questions and help you begin your journey to better health!
References:
- https://www.who.int/news-room/fact-sheets/detail/mental-disorders
- https://chriskresser.com/depression/
- Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota’s effect on mental health: The gut-brain axis. Clin Pract. 2017;7(4):987. Published 2017 Sep 15. doi:10.4081/cp.2017.987 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5641835/
- Varghese FP, Brown ES. The Hypothalamic-Pituitary-Adrenal Axis in Major Depressive Disorder: A Brief Primer for Primary Care Physicians. Prim Care Companion J Clin Psychiatry. 2001;3(4):151-155. doi:10.4088/pcc.v03n0401 https://pubmed.ncbi.nlm.nih.gov/15014598/
- Hallgren M, Kraepelien M, öjehagen A, et al. Physical exercise and internet-based cognitive–behavioural therapy in the treatment of depression: Randomised controlled trial. British Journal of Psychiatry. 2015;207(3):227-234. doi:10.1192/bjp.bp.114.160101 https://pubmed.ncbi.nlm.nih.gov/26089305/
- https://www.nimh.nih.gov/health/topics/anxiety-disorders
- https://my.clevelandclinic.org/health/articles/22513-neurotransmitters
- Terry N, Margolis KG. Serotonergic Mechanisms Regulating the GI Tract: Experimental Evidence and Therapeutic Relevance. Handb Exp Pharmacol. 2017;239:319-342. doi:10.1007/164_2016_103 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5526216/
- https://kresserinstitute.com/gut-circadian-rhythm-connection/
- https://www.sleepfoundation.org/how-sleep-works/sleep-facts-statistics
- Morin JP, Rodríguez-Durán LF, Guzmán-Ramos K, et al. Palatable Hyper-Caloric Foods Impact on Neuronal Plasticity. Front Behav Neurosci. 2017;11:19. Published 2017 Feb 14. doi:10.3389/fnbeh.2017.00019 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5306218/
- Jacka FN, O’Neil A, Opie R, et al. A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial) [published correction appears in BMC Med. 2018 Dec 28;16(1):236]. BMC Med. 2017;15(1):23. Published 2017 Jan 30. doi:10.1186/s12916-017-0791-y https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-017-0791-y
- https://my.clevelandclinic.org/health/diseases/15050-vitamin-d-vitamin-d-deficiency
- Larrieu T, Layé S. Food for Mood: Relevance of Nutritional Omega-3 Fatty Acids for Depression and Anxiety. Front Physiol. 2018;9:1047. Published 2018 Aug 6. doi:10.3389/fphys.2018.01047 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6087749/
- NaPier Z, Kanim LEA, Arabi Y, et al. Omega-3 Fatty Acid Supplementation Reduces Intervertebral Disc Degeneration. Med Sci Monit. 2019;25:9531-9537. Published 2019 Dec 14. doi:10.12659/MSM.918649 https://pubmed.ncbi.nlm.nih.gov/31836696/
- https://chriskresser.com/how-to-optimize-your-brain-for-better-cognitive-performance/

Rachel Scheer is a Certified Nutritionist who received her degree from Baylor University in Nutrition Science and Dietetics. Rachel has her own private nutrition and counseling practice located in McKinney, Texas. Rachel has helped clients with a wide range of nutritional needs enhance their athletic performance, improve their physical and mental health, and make positive lifelong eating and exercise behavior changes.
Read This Next
Micronutrients, or the vitamins and minerals your body needs, typically work like a team. To…
If you want to improve gut health, or even optimize your overall health, you’ve probably…
Have you ever found yourself grappling with the discomfort of abdominal distension, bloating, or cramping,…